Sometimes we underestimate how much of an impact practical solutions can have, even on really big problems. One of the biggest problems in Nova Scotia right now is a health care system that is in crisis. For those who feel like "crisis" isn't accurate terminology, most would at least acknowledge that we're struggling to provide enough doctors for all Nova Scotians. And, for as long as there is a shortage, we'll see the side effects.
One of the side effects is an increased number of people seeking care at our hospital Emergency Rooms for non-emergency health issues.
Keep in mind: everyday people aren't medical professionals. Only a small percentage of Nova Scotians are. There's a range of health issues for which the average person may be unable to determine if they are serious or not. As with anything, some people are better at self-assessment than others. Essentially, the average person can't confidently triage themselves - so they seek care anywhere they can find it.
Although we hear of people showing up at the ER with the flu, we also hear of people dying of pneumonia for seeking care too late. As we all know, the amount of risk a person will take suddenly becomes very low when it comes to, let's say, the parents of babies or young children, or adults with elderly family members with ongoing health issues.
Vulnerability scares us. We're afraid of not seeking help only to then discover that it's more serious than we thought.
But there's another side effect to overcrowded ERs. Over time, Nova Scotians become keenly aware of the extended wait times. The idea of being sick and waiting for hours on end - or all night - is undesirable. It can lead to a pattern of delaying seeking treatment. For those with the symptoms of the common cold, that's ok. For those with an impending cardiac arrest or seizure from undiagnosed cancer, that's not ok.
The ultimate goal is to have the Emergency Room used for emergencies and for non-emergency health issues to get appropriate attention elsewhere.
Likewise, we don't want people avoiding care, as it could mean their illness advances and puts them at greater risk or - in the most severe cases - they die from a health issue that could have been successfully treated.
So what are the basics of a practical solution?
A practical solution recognizes that very few people intend to misuse our healthcare system. A visit to their family doctor would certainly be preferred to attending a walk-in clinic or waiting in the ER. And a visit to a walk-in clinic would be, for the most part, preferred over waiting in the ER.
People want reassurance and treatment in the most convenient way possible. They want to see a doctor quickly, and (hopefully) go home to get better.
While a bigger problem may be our challenges in recruiting doctors, we can make improvements with what we have right now.
The solution is to help facilitate the flow of people seeking care to somewhere other than the Emergency Room - unless, of course, they actually have an emergency health care issue.
One way to do that is to ensure they actually know where walk-in clinics are located, with up-to-date dates and times of operation.
If people have this information readily available, they'll use it.
Don't we already have this information?
No, we don't.
- The Nova Scotia Health Authority and the 811 websites do not provide this information. The Doctors Nova Scotia website had this information in the past, but no longer has it available.
- If you call 811, the automated system doesn't provide this information. When you ask the operator for it, they tell you they cannot provide it and ask you to schedule a call back with a nurse. This has a typical wait time of approximately 30 minutes.
- If you search Google, the results are hit and miss. Some local walk-ins may turn up. Some third party sites appear with sparse and incomplete information.
For people who go to the same clinic regularly, as long as the clinic remains open, it will be reliable for them. For people who have doctors, but cannot get an appointment, the administrative assistants may have some recommendations for local walk-ins. It's also possible to track down some suggestions from other sources, such as local hospitals by telephone or even local pharmacists. These people may be asked frequently enough that they tend to know where clinics are operating.
If people do enough calling, searching, and asking around, they'll eventually come up with a local walk-in clinic.
But therein lies a bottleneck. The last thing people should have to do is call, search, and ask around when they need help. In fact, we know what many of them do instead. If they don't know where a walk-in clinic will be available soon, they may end up at the Emergency Room.
And that's how poorly designed processes that don't take into consideration how regular, everyday people make decisions add further stress on our system.
The Nova Scotia Health Authority needs to track the availability of walk-in clinics and update their changing locations, and days of the week and times of operation, every day.
I'll provide the bullet points on a more detailed solution:
- The NSHA hires a small team of administrators (the "walk-in team") that should be comprised of an experienced administrator, and several university-level paid student interns.
- This team's job is to maintain up-to-date information on every walk-in clinic in Nova Scotia and to make sure that information is distributed and promoted.
- A website is created. It allows operating walk-in clinics to register, and (once in the system) they must update their opening days and hours of operation (and additional helpful info) each time it changes.
- Participation in this system will be made mandatory for all walk-in clinics.
- The walk-in team will be auditing the walk-in clinic database to ensure that up-to-date information is being provided, and will follow up with the clinics when it is not. The system flags those with infrequent updates.
- A public website for walk-in clinics only is created at 811.novascotia.ca/walkins.
- The main 811 website has a large orange button at the top of the page stating [ Find A Walk-In Clinic ]

- The same button is added to the top of the www.nshealth.ca website.
- The site offers the capability for other healthcare providers to add the button to their websites to help promote it.
- The 811 operator has access to the website. A 3rd option is added to the phone line: "Help me find a local walk-in clinic". When the option is selected, the operator verifies their town/city and informs them of the walk-in clinic availability nearby for the next few days. The operator offers to (i) email, or (ii) SMS text message this information, and provides them with the website if they have Internet access via a smartphone or computer.
- The walk-in team promotes the new website to all medical facilities, ERs, individual doctors, nurse practitioners, and pharmacists to empower them all to be able to provide accurate information whenever asked.
- Upon request, anyone who registers can be notified by email whenever one of their local walk-in clinics has a change in operating days or hours, or if a new clinic opens in the same area. This ensures that they are alerted of this information without having to keep checking for updates on days when there are none.
- Large posters to promote the website are distributed to every ER, doctors office, and healthcare facility in the province. Anyone can request a copy of the poster online if they have a location where many members of the public congregate and wish to provide a public service. The walk-in team will follow up after they are sent to ask each facility if they have displayed the poster.
- Business cards are printed that promote the new service. The information is minimal and focused. One side says: "For non-emergency healthcare needs, call your doctor or find a walk-in clinic at 811.novascotia/walkins" The opposing side says "Call 811 for health information. Call 911 if you have a medical emergency". The cards are provided to every Emergency Room triage nurse in the province's ERs. They are required to give them to any patient who has arrived with a non-emergency health issue so that they'll be aware of the information when future health-related concerns arise.
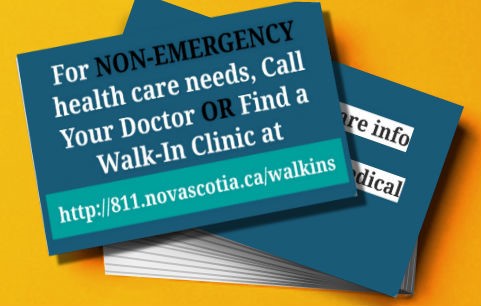
- The walk-in clinic promotes the business cards to pharmacists in the province and requests that they agree to either insert them into prescription packaging or display them on a business card holder at the pharmacists counter. People with health issues appear at these counters frequently, and it's an excellent place to promote the new walk-in clinic website (or its information via a call to 811).
That is the basic details of a cost-effective solution of ensuring walk-in clinic information is always up to date and readily accessible to everyone in the province. If they can find a walk-in easily, they are more likely to seek care at one, and less likely to use an Emergency Room as the place of last resort.
By collecting data of the peak times of people seeking care at Emergency Rooms, and comparing to the data collected about the days and hours of operation for local walk-in clinics, the NSHA will be able to identify times when there's insufficient walk-in availability.
The walk-in team can then report this data concisely and provide it to walk-in clinic operators in the areas to ask that they offer opening hours to take the stress off of the ER. The report may also encourage doctors not yet operating walk-in clinics to consider the opportunity to do so.
For example, if there were no walk-ins or doctors open after 5 pm on a particular day, and a person develops a medical concern that makes them believe they need care that evening, they are going to end up at the Emergency Room. The only way to avoid that is to (a) have walk-in clinic availability during those hours, AND (b) make sure people actually know where to find one.
This has been a long description, with a bunch of bullet points. But the basics of the solution is practical and cost-effective. It is designed to think about how regular, everyday people navigate our healthcare system, and how we can optimize that flow.
Ultimately, a poorly managed flow in the healthcare system leads to many more adverse side effects. It's always in our best interest to make the kinds of improvements that are within our abilities.
A healthcare system that doesn't recognize the opportunity for practical solutions just demonstrates why it finds itself in a crisis situation in the first place. Sometimes we most certainly underestimate how much of an impact practical solutions can have, even on really big problems.
NOTE: The views expressed above are my own and do not represent lokol (goCapeBreton.com). Read more






7
Log In or Sign Up to add a comment.- 1
arrow-eseek-e1 - 1 of 1 itemsFacebook Comments